Even while our skin frequently gives away information about our general health and happiness, it occasionally throws us for a loop. One such difficulty is the emergence of Milialar, also called “milk spots” or “oil seeds.” These tiny, frequently white or yellowish pimples can be highly upsetting for people who come into contact with them. We’ll go into the world of Mililar in this post, learning what they are, why they happen, and how to handle them.
What Does Milialar Mean?
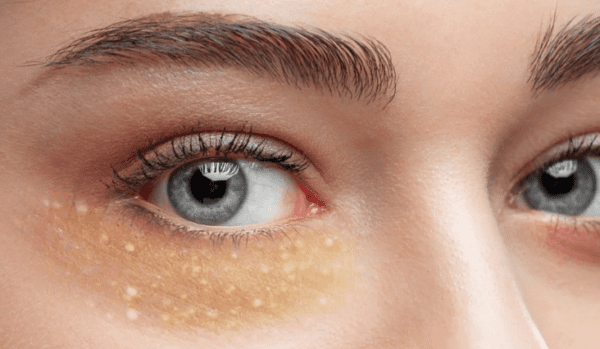
Small, painless cysts that appear on the skin as white or yellowish lumps are known as mililars. They are resistant to traditional squeezing or popping because, unlike acne, they don’t have an opening or pore. Dead skin cells getting stuck just below the skin’s surface is what causes these pimples.
Identification of Milialar: Signs and Symptoms
Size and Color Differences
They resemble small pinhead-sized skin pimples. They resemble tiny pearls or seeds and are available in white or yellowish tones. These differences in size and hue are typical features of the familiar.
Locations Often Found on the Body
Although it can occur anywhere on the body, it seems to favor certain locations. The face, particularly the area around the eyes and cheeks, is where they appear most frequently. But they can also be observed on the forehead, nose, and — rarely — the upper body.
Issues that could arise
Military as a whole are often benign and don’t hurt or bother anyone, but they might be an aesthetic issue. In some situations, such as when exposed to strong sunshine, they might stand out more or last longer, which could cause aesthetic problems.
Causes of it
Miliar development is influenced by several variables, including:
Newborns
It is uncertain what causes milia in babies. It is frequently confused with baby acne, which is brought on by maternal hormones.
Milia does not result in edema or inflammation, in contrast to infant acne. Baby acne doesn’t show up until two to four weeks after delivery, although milia is typically present from birth.

Older adults and kids
Milia in older children and adults is usually linked to some kind of skin injury.
This could involve:
blistering brought on by a skin ailment like porphyria cutanea tarda (PCT), cicatricial pemphigoid, or epidermolysis bullosa (EB)
scorching wounds like poison ivy
fires
persistent solar damage
long-term steroid cream usage
techniques for skin resurfacing, like laser or dermabrasion resurfacing
Overproduction and trapping of keratin:
- Excess keratin, a protein found in the skin, can get trapped beneath the skin’s surface and cause milia to grow.
Damage to oil glands or sweat ducts:
- Oil glands and sweat ducts in the skin can become damaged by trauma, such as burns or sun exposure.
- Tiny cysts packed with oil and dead skin cells from blocked ducts or glands can develop into milia.
Products for skincare and cosmetics:
- Some cosmetics and skincare products, especially thick creams and moisturizers that aren’t right for your skin type, might clog pores and perhaps lead to milia.
Genetics:
- Certain people may be more prone to developing milia due to genetic predisposition.
- A family history of it can increase the likelihood of this problem occurring.
Age Factors for Armed Forces
Our skin changes with age. This includes skin disorders such as milia. Although milialar can afflict anybody, its development may be influenced by circumstances connected to age.
One factor is aging naturally. Our skin loses its ability to efficiently eliminate old cells and renew new ones as we age. Keratin may therefore become trapped under the skin’s surface and appear as milia-like lumps.
Sun exposure is a further issue related to aging. Prolonged sun exposure destroys the collagen and elastin in the skin. Milia and a delay in cell regeneration might arise from this.
Changes in the amounts or imbalances of menopausal hormones may impact oil production and raise the risk of milia.
Smoking and poor diet can worsen pre-existing conditions or make treatment more challenging.
Recognize and handle family problems at any age by knowing these age-related traits!
Medical Diagnosis and Evaluation
Typically, a dermatologist or other specialist healthcare provider makes the diagnosis of milia. They carefully scrutinize the size, form, and color of the lumps as they undertake a comprehensive visual examination of your skin. For a closer examination, they occasionally use magnification equipment like a dermatoscope.
For a thorough assessment, your medical background, medication use, and skincare products are also taken into account. If there is any doubt, a microscopic examination may done on a small tissue sample (biopsy) taken from one of the pimples. A precise diagnosis is necessary for individualized milia treatment. Self-diagnosis is discouraging because various skin disorders might resemble milia, highlighting the value of expert assessment and direction.
Milialar Treatment Options
Depending on their size, location, and persistence, the management of it may vary. Typical forms of treatment include:
Automatic Resolution: This condition may often go better without any special care.
Cosmetic dermatology procedures: Dermatologists can eliminate warts using cryotherapy, laser therapy, chemical peels, and microdermabrasion.
Retinoids used topically: Topical retinoids, whether prescribed or over-the-counter, can occasionally aid in the eradication of milia.
Home Treatments: Home remedies like gentle exfoliation and adequate skincare regimens can help manage and prevent the development of milia.
Prevention and at-home remedies
This article will offer natural remedies and preventative methods for coping with and lowering the risk of the following:
- By taking precautions regarding sun exposure, such as wearing clothing or sunscreen whenever possible, vulval milial cysts can avoid.
- Benzoyl peroxide, salicylic acid, as well as lactic acid, are three over-the-counter drugs that are beneficial in reducing the appearance of milia.
- Oral Antibiotics: A doctor may suggest using an oral antibiotic like doxycycline or amoxicillin if the sickness is serious enough.
Conclusion
Even while Milialar is mostly harmless, it can be an aesthetic problem or make some people uncomfortable. The entire spectrum is addressed in this manual, including its causes, treatments, and prevention strategies. To determine the best course of treatment for persistent or bothersome vulvar milial cysts, a dermatologist consultation advised. By following proper skincare habits and utilizing the right protection, miliary development can stop and clean skin can retain.
FAQ’
Do similar things hurt?
No, it usually doesn’t hurt. They are less a source of pain physically and more of an aesthetic issue.
Can I pop pimples that look similar to them?
The condition does not have an opening or pore, so attempting to pop one could irritate the skin and perhaps cause infection. It’s important to get help from an expert.
Do miliarial disappear on their own?
On occasion, it may spontaneously disappear without any medical intervention. However, under rare circumstances, they might endure for a long time.
What Milialar therapy alternatives are available?
Milia is treat with chemical peels, topical retinoids, professional extraction by dermatologists, and exfoliation. The nature and severity of the Milia will determine the therapy option.
Are there any Milielar home remedies?
Although some individuals may attempt homemade therapies like warm compresses, it advise to see a dermatologist for an accurate diagnosis and course of therapy.